
Michael Murphy on the Architecture of Health
It has been a surprisingly rapid ascent for MASS Design Group. Famously founded in 2008 by Michael Murphy and Alan Ricks, a pair of Harvard Graduate School of Design students, the firm made an immediate name for itself with its first project, the Butaro District Hospital in Rwanda. Built on a low budget and with local workers, the naturally ventilated clinic created both a new healthcare paradigm in Africa and a fresh business model for designers interested in a different way of practicing. (MASS stands for “Model of Architecture Serving Society.”)
Based in Boston, Massachusetts, and Kigali, Rwanda, the nonprofit firm is now 200 strong and includes architects, planners, engineers, landscape architects, furniture designers, writers, and filmmakers. Last week was a big one for MASS. The American Institute of Architects named it the 2022 Firm of the Year. At the same time, the Cooper Hewitt, Smithsonian Design Museum debuted Design and Healing: Creative Responses to Epidemics, an exhibition organized by the firm, and released a comprehensive accompanying book on the history of hospital design entitled The Architecture of Health, written by Murphy and MASS colleague Jeffrey Mansfield. Prior to the AIA announcement, but after the firm’s profile on 60 Minutes, I talked to Murphy about the book, the state of hospital design, and why healthcare is not part of the architectural canon.
MCP: Martin C. Pedersen
MM: Michael Murphy
Let’s talk about The Architecture of Health. Give me some of the backstory on it.
We’ve been working on a version of this for about six years. The seed for it was planted during the first project we worked on in Northern Rwanda, with Partners in Health. The idea was these buildings had to be designed to directly address the health outcomes of the patients in them. The particular challenge there was the movement of airborne disease. We went into that project asking a series of questions about how buildings shape health. We studied the history of hospitals and discovered that over the course of the last century and a half, buildings have been at the forefront of trying to address how we can live in more healthy ways and reduce disease, infection, and illness, through the advancement of architecture.

It seems, though, we got stuck. Hospital design, at least in the U.S., advanced to a certain point, and then didn’t really evolve a lot from the ’70s and ’80s. Now there’s a long-overdue shift. But there was a fairly long period of statis, because of codes, air handling, even lawsuits.
That’s an important point. Almost a hundred years after Florence Nightingale’s Notes on Hospitals, we faced this next paradigm shift. With the advances in medicine, the complexity of surgery and medical care, the increase in litigation around hospital-borne infections, the hospital became a medical machine. But I think the utopian thinking of the ’60s architectural profession helped advance this idea, too. After the war, we have these big visions of healing, doing something dramatic with these large floor plates that can now be mechanically ventilated.
And then in America it became coupled with urban planning, because these facilities were so big, they tended to be medical districts rather than discrete buildings.
That’s exactly right. We talk about this in the book. I am really interested in this period in the ’60s when hospitals got big. Reyner Banham theorizes about the megastructure and says there aren’t that many megastructures that were truly realized; they were more theorized.
Thank god.
Exactly. But the megastructure as theorized by Banham emerges as the hospital. To some degree, it makes sense because the hospital at its core is the best example of a kind of living architecture—it’s always under construction, always being added to and amended. And so this Frankenstein-esque result is this living thing. Its inability to stay a static object is also why it’s often under-theorized, because it’s so much easier to look back at architecture of one type and say, “This is what so-and-so was thinking at this period of time, and isn’t that amazing?”
Medical campuses do have a lot of layering. Often, there’s a ’70s building next to the turn-of-the-century building. There might even be a 19th-century, former surgical amphitheater somewhere in there.
And each one of those buildings had their own logic that tried to answer the question: How does this space affect health? When the Covid epidemic struck, we did research for Mount Sinai Hospital in New York. It turns out the more modern buildings, the ones built in the ’70s and ’80s, one designed by I.M. Pei, for example, had inoperable windows.
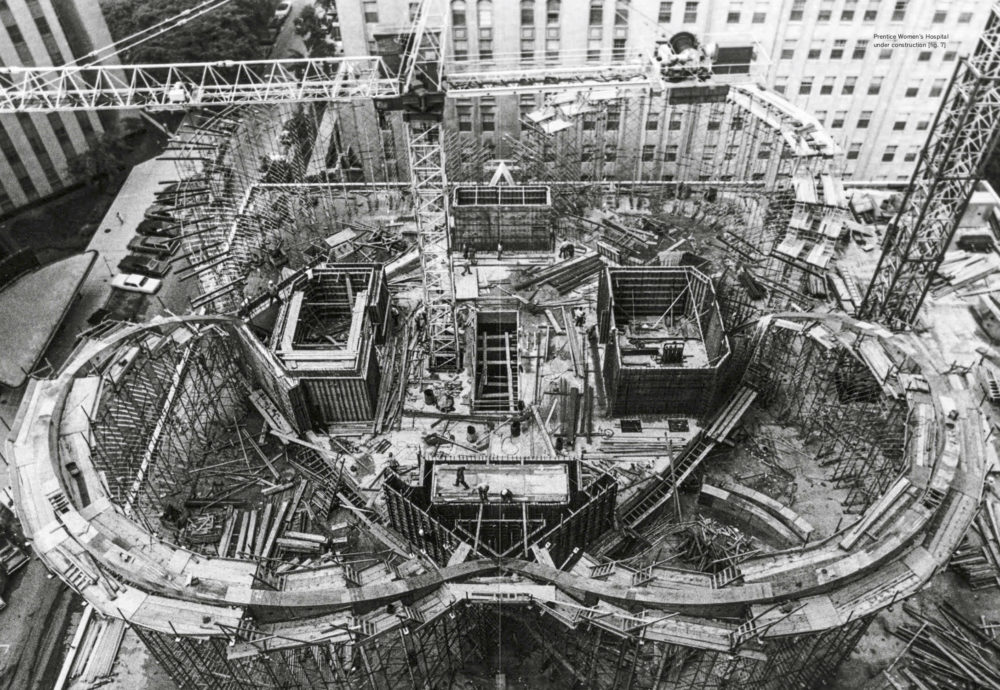
Prentice Women's Hospital, in Chicago. Designed by Bertrand Goldberg, it was demolished in 2013.
Sealed boxes.
They wanted to control the indoor air. That was the hypothesis. So Sinai turned the old bed towers from the 1920s, which had operable windows, into Covid units because they could more easily adapt them to airflow needs. I find that a fascinating and revelatory hack. It was the introduction of mechanical systems that allowed that leap in scale to happen, where the floorplate could extend a whole block. But it created a much more vulnerable system, one that was unadaptable to things like an epidemic.
Your architectural journey started in healthcare, in Africa. What first principles did you bring from that early project into newer healthcare projects here?
We were looking for principles that are adaptable anywhere. One is that buildings have to breathe. This applies to any building anywhere. When we look at who suffered the most during the epidemic, it was nursing homes and carceral facilities. Places where people couldn’t leave or didn’t have the ability to manage their own environments. That’s an example of where buildings failed. If buildings are keeping us from breathing fresh air, then they are fundamentally keeping us from accessing a core right to life. We learned in Northern Rwanda that buildings deeply impact the ability to access our rights as citizens. It was not just without providing healthcare. It came down to: Does the building also function in a way that supports these bigger ideals of dignity creation, citizenship, equity?
And buildings either facilitate or impede that.
Correct. The third core principle involved beauty. In Rwanda there was a brilliant doctor who was working alongside us, a cardiac surgeon. The whole time we were working, he gave me a really hard time, asking difficult questions. It was clear that he didn’t think we were necessary. About a year after the hospital was built, he came up to me at an event and said, “I want to tell you, honestly, I thought what you were doing was a waste of time and resources, and a serious distraction from our work. I was angry that you were there. But I went to the hospital, I saw this stone wall, and realized that I was wrong. We can’t provide healthcare without providing a place that cares for the whole person. The beauty of the place transformed my understanding of why it was necessary to invest in architecture.” This doctor was coming out of a scarcity mindset, saying we have limited resources and so many people to treat. That’s the public health crisis. And yet he came to the hospital and saw that its beauty mattered, not just to the designers, but to the patients. They talked about the stone wall, not about the airflow-management system. That was the message, the delivery method for saying that this is a place that cares for you.

Prentice Women's Hospital, from The Architecture of Health (Cooper Hewitt).
My wife is a doctor, so I’ve spent too much time in hospitals. I get frustrated in American hospitals. I’ll walk into the lobby and see that’s where the “design” happened. The glass curtain wall makes a nice statement. I’m not against beautiful hospital lobbies—I appreciate them. But then I go through the doors and get into the machine, and it becomes about solving mechanical problems.
I couldn’t agree more. It’s like they do the lobby, design the big foyer, and then everything else feels generic and off the shelf. If you go through the history, there’s always been a search for the solution. You go back to Corbu’s Venice Hospital, or even some of the Situationists, or think about the Free University of Berlin, where there’s this interior environment that could spark curiosity and joy, while you’re lost in the system.
Well, if you’re in a hospital, you’re inevitably going to be lost. And the wayfinding is either going to be good or bad.
It’s fascinating. The modern hospital really emerges out of a number of Utopian ideas, but the eventual outcome is the very opposite of that: it’s institutionalized; it’s feeling deeply lost; the labyrinth is quite dehumanizing. The hallways, the banality of physically traversing the medical system in the United States—what better analog to how labyrinthine and difficult to traverse our medical system is than the hospital building itself.
It is actually a perfect reflection.
A perfect built manifestation of the system it represents. And I think the way out is to thin buildings out again, make them breathable, directly related to their environments. The indoor/outdoor is what Dan Barber recently talked about in his amazing book, Modern Architecture and Climate: Design Before Air Conditioning. Hospitals have to be more connected to air and light, to the experience and the journey of the individual. Now, I’m not saying it should be the end of mechanical ventilation. Of course there’s going to be mechanical ventilation, but a more mixed-mode or resilient system is absolutely essential.
How much of MASS’s work is healthcare?
It was where we began, and we’ve continued to do it. It’s a big piece of our portfolio. I’d say now it’s probably 15% to 20%. But we’ve grown. We’re doing a lot of work in memorials and spaces of memory, the public realm.
The Memorial for Peace and Justice in Alabama was spectacular. The best memorial that I’d seen in decades.
It was amazing to be able to work on that. We’ve got a new memorial in Boston Common to Martin Luther King and Coretta Scott King. We’re doing a number of housing projects, affordable housing, across the U.S., and then we’re doing a lot of work in my hometown, Poughkeepsie, New York.
I saw that on 60 Minutes.
That’s more at an urban scale. So it’s everything from this new headquarters for a nonprofit to a large park system. The typologies have grown. We’re agnostic about typologies.

The co-founders of the MASS Design Group, Alan Ricks (left) and Michael Murphy.
You started being very agnostic about typologies when you leapt into a famously untrendy building type.
Hospitals were not the buildings that we studied in architectural history. Healthcare design was considered a subdiscipline. It wasn’t part of the canon. I think that one of the real purposes of this book is to say, “We have to consider the hospital in order to understand the history of architecture.” It’s a kind of uber-architecture, because it asks all of the fundamental questions that we must ask of buildings.
I think MASS marked a culture shift within architecture. It emerged at the end of the age of overt formalism. The firm helped shift the profession away from the museum being the be all and end all of formal expression.
I appreciate you saying that. I often think about that period of time. We didn’t set out to do anything of that type.
You would have failed if you’d set out to do it.
I think about what was in the water, what was happening then. The Rwanda project began at the crux of the Great Recession. When we started the work, everybody was losing their jobs, and somehow I was getting a job in this place where no one thought there was any work. And then we had to answer tough questions from medical professionals who were suspicious about our value, who said: Prove to me that this will improve the health of the patients; prove to us that there’s some logic behind these decisions that improves the performance of doctors in the medical space.
That kind of rigorous engagement forced us to defend some core principles of architecture, all the way through the process. There was also this brewing movement that you’ve followed and written about, from Sam Mockbee to Bryan Bell to Architecture for Humanity and others. From the late ’90s to the early aughts, there was a visible undercurrent of a more responsive social and environmental architecture. It was being theorized as an “alternative.” There was capital A architecture, and then there was this other thing, healthcare. We were in the middle of that, but I always felt uncomfortable with the idea of being a subdiscipline.
I remember you would always say, “No, no, we want to be part of the discourse.”
I thought it was important, because looking historically you see that the same debate reoccurs. At each one of these junctures, there’s a desire in the profession, from William Morris to Giancarlo DeCarlo, to have some accountability for the social, environmental, and physiological impacts of design. But in the case of the hospital, there is no debate about whether buildings can or should impact behavior and health. That debate is not happening with doctors. So I find it really helpful to go back to the hospital, where that design debate doesn’t exist—because it can’t exist for the hospital to work. It also helps pull us out of this false dichotomy about whether we’re social architects or capital A architects. That’s a false binary. We are both. One is a process, the other is an end.
Featured image of the Butaro Hospital by Iwan Baan.
